Antibiotics overuse raises threat
Updated: 2016-09-23 07:59
By Shan Juan(China Daily Europe)
|
|||||||||
A British report estimates that antimicrobial resistance could cause 1 million premature deaths a year in China by 2050
Imagine you have bacterial infection and all the antibiotics prescribed by doctors cannot cure it. This is no sci-fi scenario about superbugs but is actually happening worldwide. Improper or overuse of antibiotics is the leading cause of public health problems.
China accounts for half of the antibiotics consumed worldwide, half for humans and the rest for livestock. Antibiotics have long been available in hospitals to prevent post-surgery infections and other infections. They are also available over the counter at drugstores, which people use to treat coughs or a running nose.
Public health experts say the more antibiotics a person has taken, the greater the threat he or she faces from superbugs. They have called for strengthened and coordinated government efforts to address the challenge.
The Review on Anti-microbial Resistance, a report published in Britain this year, estimates that AMR, including antibiotic resistance, could cause 1 million premature deaths a year in China by 2050.
Chinese policymakers have recognized the looming crisis and decided to take coordinated action. A state-level action plan on AMR prevention and control will be issued this month by more than 10 departments, including the National Health and Family Planning Commission, the Food and Drug Administration, and the education and agriculture ministries.
Xiao Yonghong, a professor at Peking University's Institute of Clinical Pharmacology, says the long overdue initiative shows the government's determination to tackle the issue head on.

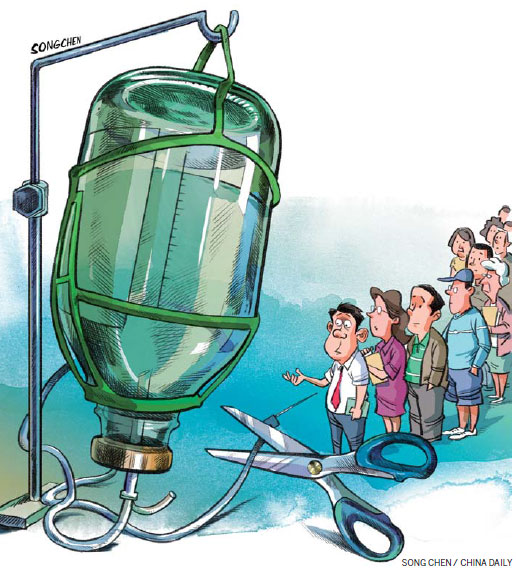
Previously, the health authorities largely initiated measures to fight AMR, which included stricter control of antibiotic usage at medical facilities. For instance, last year, Jiangsu became the first province to issue a blanket ban on the use of intravenous antibiotics on outpatients. Provincial health authorities say the ban is working, with public awareness about overuse of antibiotics increasing.
Other provinces such as Zhejiang, Jiangxi and Anhui are likely to follow suit. But that's still far from enough.
The misuse of antibiotics in the agricultural sector is still widespread, as noted by many Chinese experts and the British report on AMR.
To prevent infections and to boost growth, farmers regularly feed antibiotics to their livestock. This has turned farms into fertile breeding grounds for drug-resistant pathogens that could also threaten humans. Remember a joint China-US study in 2013? It found "diverse and abundant antibiotic-resistant genes in Chinese pig farms", which could contaminate the soil and water and migrate to humans through food.
So the fight against AMR cannot be won without the active involvement of the agriculture sector, for which the use of antibiotics must be drastically curbed.
Other stakeholders like the environment and education authorities, too, have to join the fight by monitoring the antibiotics contamination level and helping to raise public awareness.
There's still a long way to go, and the expected government action plan will be a good start to the all-out war on AMR in China. That will also help China fulfill its international responsibility in public health.
Previously, cross-border medical tourism was blamed for the spread of NDM-1, a bacteria-resistant enzyme, after a British national visiting India for low-cost surgery carried the superbug home. However, nonmedical tourists from the United States also carried the superbug home from India.
Be that as it may, with one-fifth of the world's population, China has to be part of the global fight against AMR. The war on AMR cannot be won without China.
The author is a senior reporter with China Daily. Contact the writer at shanjuan@chinadaily.com.cn
(China Daily European Weekly 09/23/2016 page12)
Today's Top News
State of emergency declared in US city amid protests
Universities given boost in rankings
Demand for Mandarin rises in UK
China 'capable of keeping medium-to-high growth'
Li tells Obama of opposition to THAAD deployment
Greek vows to improve refugee situation on island
UN suspends aid convoys following deadly strikes
New York bombing suspect captured in New Jersey
Hot Topics
Lunar probe , China growth forecasts, Emission rules get tougher, China seen through 'colored lens', International board,
Editor's Picks

|

|

|
|

|
|